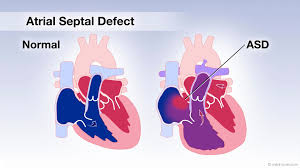
 Atrial septal defect (ASD) is a hole in the wall between the two upper chambers of the heart (Atria). As a result, some blood from the left atrium is diverted to the right atrium. There is consequent increase in the blood flow into the right ventricle and these two chambers of the heart get enlarged. Untreated, there can be long term consequences on the heart and the lungs. This defect is congenital – i.e., present from birth.
Atrial septal defect (ASD) is a hole in the wall between the two upper chambers of the heart (Atria). As a result, some blood from the left atrium is diverted to the right atrium. There is consequent increase in the blood flow into the right ventricle and these two chambers of the heart get enlarged. Untreated, there can be long term consequences on the heart and the lungs. This defect is congenital – i.e., present from birth.
The defect is often detected during a routine clinical examination or an Echocardiogram. Nowadays, antenatal ultrasound examination of the baby while it is in the mother’s womb termed as the Anomaly Scan, can potentially detect such defects even before birth. Moreover, a widespread availability of Child Specialists across the country ensures detection in early childhood in the twenty-first century. Most patients with ASD do not have symptoms until middle age. However, as the pressure on the right side of the heart increases with age, some may have shortness of breath or feeling of irregular heartbeat (palpitations), tiredness, swelling in the legs and even stroke as a complication of irregular heart beat. Therefore, early detection and treatment before any of these problems arise is recommended.
Based on the symptoms, size and pressure changes in the heart, these defects can be either left alone or closed. Smaller holes may close on their own in childhood. However, medium to large-sized ASDs may need closure by device or surgery.
Smaller holes especially the common variant called Ostium secondum (OS-ASD) can be closed non surgically by a device closure method. (Device closure of ASD Read here). Complex ASD (sinus venosus, ostium primum), multiple defects or larger holes are closed surgically.
Hole in the heart: Atrial septal defect
A 11-year-old girl was brought to the hospital for a cardiac evaluation by her parents. She was told to have a ‘heart murmur’ during her annual health examination at school. She was asymptomatic and quite active. Her parents had not noticed any complaints like breathlessness, chest pain, palpitations or difficulty to gain weight.
On clinical examination, she was found to have a cardiac murmur (abnormal sound in the heart). This led to a strong suspicion of a ‘hole in the heart’. Echocardiography was performed and it confirmed the presence of a hole in the wall separating the right and the left atria, upper chambers of the heart. This hole is medically referred to as Atrial Septal Defect (ASD).
 Initial tests were surprisingly normal. As per standard guidelines, in view of cardiac arrest patient was advised a coronary angiography test. Initially the family members were reluctant to subject him for this test due to his age.
Initial tests were surprisingly normal. As per standard guidelines, in view of cardiac arrest patient was advised a coronary angiography test. Initially the family members were reluctant to subject him for this test due to his age.
However, as the patient was otherwise physically fit, was of sound mental health and his quality of life was good, the family decided to get the coronary angiography done for the patient. Two critical blocks in the major coronary arteries were detected.
The blocks were treated non-surgically with coronary stents with minimum discomfort to the patient. He was discharged within 48 hours of arrival to the hospital. He has since then been on follow up for last 8 months and is doing well.
The commonest cause of Cardiac arrest in any age group is a heart attack or block in coronary arteries. When a patient suffers a cardiac arrest outside a hospital, prompt CPR is lifesaving; a skill that most citizens should learn. Survivors of cardiac arrest should undergo coronary angiography to detect and treat blockages in the coronary arteries.
Example: An 84 years old gentleman, with no prior medical history, collapsed in his home while sitting. Luckily, his neighbour who happened to be a Paediatrician, was alerted immediately. The doctor rushed to the patient’s home, realised that this was a cardiac arrest, performed cardiopulmonary resuscitation (CPR) and revived him within 5 mins. He was then brought to our hospital and assessed in the Emergency Room.
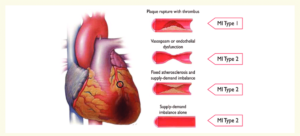
 A 65-year-old PhD went for a trek to Tiger Hills, known as a very tough climb in Bhutan. He was not on any regular exercise training program and had not prepared himself for this trek adequately. After the climb to the hill summit, he experienced severe chest discomfort and burning in the front of the chest. He attributed it to the changed food habits while on the tour and returned the same day to India as planned. After he landed in Bangalore airport, he directly came to our hospital due to further increase in the chest discomfort.
A 65-year-old PhD went for a trek to Tiger Hills, known as a very tough climb in Bhutan. He was not on any regular exercise training program and had not prepared himself for this trek adequately. After the climb to the hill summit, he experienced severe chest discomfort and burning in the front of the chest. He attributed it to the changed food habits while on the tour and returned the same day to India as planned. After he landed in Bangalore airport, he directly came to our hospital due to further increase in the chest discomfort.
Upon arrival to the emergency he was diagnosed to have a heart attack by ECG and other tests. He was taken into the cardiac catheterisation lab and an emergency angiography was performed. One of the major coronary arteries was blocked and he also underwent an emergency coronary angioplasty. It was also noted that there was a second block in another artery that would require another angioplasty after 6 weeks. After satisfactory recovery, patient was discharged with advice to return for the second procedure.
As Covid pandemic set in, patient did not turn up for the next procedure. Unfortunately, he had another heart attack this time involving the second block. Luckily, he presented early to hospital and an emergency coronary angioplasty was done for the other narrowing as well. He is doing well with more than 9 months follow up.
Take home lessons:
- Unaccustomed, strenuous physical activity can lead to plaque rupture (link this to a FAQ) and heart attacks. Always follow graded exercise regimen before sport or recreational activity involving physical strain.
- Discuss with your physician the pros and cons of postponing essential medical procedures.
 A 35 year old man, movie singer by profession, a known smoker developed severe chest pain in our hospital while accompanying a relative for treatment. He was rushed to the emergency department. An ECG was performed which revealed that he had suffered a heart attack. Emergency medications were administered and further treatment was discussed with the patient and family.
A 35 year old man, movie singer by profession, a known smoker developed severe chest pain in our hospital while accompanying a relative for treatment. He was rushed to the emergency department. An ECG was performed which revealed that he had suffered a heart attack. Emergency medications were administered and further treatment was discussed with the patient and family.
After that the patient was shifted to the cardiac catheterization lab. He was subjected to an emergency Coronary Angiography test which revealed ta block in the ?WHICH ARTERY. Immediately, Primary Coronary Angioplasty (a procedure to urgently relieve the block and restore blood flow in obstructed artery) was begun.
Even as the procedure started the patient had Cardiac Arrest (stoppage of heart) due to an abnormal rhythm called Ventricular Fibrillation. This was immediately treated with an Defibrillation, delivery of electrical shock to the heart and normal heart rhythm was restored. The Primary angioplasty procedure was continued and block in the artery was cleared followed by insertion of a coronary stent (Hyperlink to FAQ question “What is a Stent?”).
Patient made complete recovery and was discharged after 48 hours. He is on a regular follow up having quit smoking and changing his lifestyle and diet
Irregular heart rhythms such as Ventricular tachycardia (VT) and ventricular fibrillation (VF) are the commonest reasons for sudden death during a heart attack. VT/VF that happen within the first 24 hours of a heart attack are called Primary VT/VF. Those that happen later are called secondary VT/VF.
Primary VT/VF are due to blocks in the coronary artery and consequent lack of oxygen to the heart muscle. These are treated with Electrical shock and by relieving the blocks early as was done in our case. Secondary VT/VFs are due to damaged heart muscle due to delay in appropriate treatment of heart attacks and are far more tougher to treat.
Therefore the key priniciples in treating sudden cardiac death in a heart attack is early treatment of heart attack to reverse Primary VT/VF and prevention of heart muscle damage to avoid secondary VT/VF
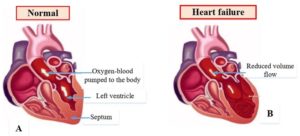 A 56-year-old male was brought to the Emergency with history of sudden onset shortness of breath since one day. He gave a history of shortness of breath while walking uphill and climbing stairs since one month. There was no chest pain or sweating. He was also uncomfortable while sleeping and was using around three pillows for the same. He had noticed swelling of both feet and decreased urine output since 2 weeks. The family had noticed that his appetite had decreased but he was gaining weight.
A 56-year-old male was brought to the Emergency with history of sudden onset shortness of breath since one day. He gave a history of shortness of breath while walking uphill and climbing stairs since one month. There was no chest pain or sweating. He was also uncomfortable while sleeping and was using around three pillows for the same. He had noticed swelling of both feet and decreased urine output since 2 weeks. The family had noticed that his appetite had decreased but he was gaining weight.
On examination, there was swelling of both feet, his neck veins were engorged, and he was unable to lie down flat. A clinical diagnosis of ‘Acute heart failure’ was made.
ECG ruled out an acute heart attack. Chest Xray showed presence of fluid in his lungs. 2DECHO confirmed the presence of heart failure. His heart pumping (LVEF) had reduced and the pressure inside the heart chambers was also increased.
This condition is called Acute heart failure with reduced ejection fraction or Congestive cardiac failure. He was then immediately started with IV medications to help reduce the fluid from the body. Oral medications to improve his heart rate and pumping were advised.
Once he was stabilised, coronary angiography was suggested to rule out blocks in the blood vessels (coronary arteries) of the heart. There was a 90% blockage in his Left anterior descending (LAD) artery which was cleared by a coronary angioplasty.
Heart failure means that the heart isn’t pumping as efficiently as it should. It does not mean that the heart has stopped working. The heart muscle is sometimes too weak and cannot pump blood to the rest of the body with enough force (systolic failure). Sometimes it becomes stiff and has trouble in relaxation and can’t fill with enough blood (diastolic failure). Systolic and Diastolic heart failure can also co-exist. Patients with heart failure may require medicines and other forms of treatment to help the heart function better and to remain free from symptoms.
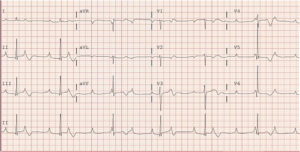 A 74-year-old female came to the emergency with complaints of extreme tiredness and dizziness since two days. She had a history of diabetes and hypertension for more than a decade. She denied any chest pain, shortness of breath, ringing sensation in the ears or loss of consciousness.
A 74-year-old female came to the emergency with complaints of extreme tiredness and dizziness since two days. She had a history of diabetes and hypertension for more than a decade. She denied any chest pain, shortness of breath, ringing sensation in the ears or loss of consciousness.
On physical examination, she was found to have a very low pulse rate (PR 36/min). Her Blood pressure was in the normal range. ECG was done which showed the presence of a Complete heart block. (Insert ECG image).
As she was symptomatic, she was immediately admitted, and a temporary pacemaker was inserted through her right groin. This is a lead/ wire which is placed into the right heart chamber (right ventricle) and then connected to a battery and the heart rate can be set at a particular value to improve the symptoms.
Complete heart block is an abnormal heart rhythm resulting from a defect in the conduction system of the heart. In this type of block, electrical signals don’t pass from the upper chambers of the heart (atria) to the lower chambers (ventricles) at all for periods of time. There is a complete failure of electrical conduction. This can result in very slow pulse leading to symptoms like giddiness, extreme tiredness and even fall and unconsciousness.
Complete heart block most often occurs in the elderly due to degeneration of the conduction system of the heart. Other reversible causes like electrolyte disturbances (variation in sodium, potassium levels), abnormal thyroid levels, excessive dose of medications (beta blockers) can also cause the same.
Treatment depends on the cause. If the cause is reversible, treatment should be focussed on the same (Eg: correction of potassium levels). If it is degenerative in nature, a ‘Permanent Pacemaker’ implantation is advised. (Insert Permanent pacemaker image/ link)
A permanent pacemaker is a device that is implanted under the collar bone which helps in controlling the heart rate and helps the heart beat more regularly.
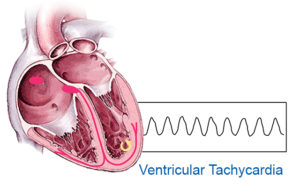 A 60-year-old patient presented to ER in the noon with severe chest pain from 1 hour along with his son. In ER, ECG was taken and diagnosed as acute anterior myocardial infarction. Cardiologist was alerted right away who came down to talk to the patient. While taking the patient’s history, he had a cardiac arrest with ventricular tachycardia (abnormal rhythm). He was DC cardioverted with rhythm returning to normal. He was taken up immediately to cathlab after discussing with the attenders and consent was obtained for the procedure after explaining risks briefly. In cathlab, high risk Primary coronary angioplasty, a minimal invasive procedure of stent insertion into the occluded artery of heart was done along with special mechanical circulatory support procedure known as Intra-aortic balloon pump (IABP) was also inserted during the procedure to support the heart. Procedure was completed successfully without any further issues. IABP support was slowly reduced and removed after 4 days. After an extended stay in hospital, patient was discharged and went home. He is doing well after 1 year of follow up without any further cardiac issues.
A 60-year-old patient presented to ER in the noon with severe chest pain from 1 hour along with his son. In ER, ECG was taken and diagnosed as acute anterior myocardial infarction. Cardiologist was alerted right away who came down to talk to the patient. While taking the patient’s history, he had a cardiac arrest with ventricular tachycardia (abnormal rhythm). He was DC cardioverted with rhythm returning to normal. He was taken up immediately to cathlab after discussing with the attenders and consent was obtained for the procedure after explaining risks briefly. In cathlab, high risk Primary coronary angioplasty, a minimal invasive procedure of stent insertion into the occluded artery of heart was done along with special mechanical circulatory support procedure known as Intra-aortic balloon pump (IABP) was also inserted during the procedure to support the heart. Procedure was completed successfully without any further issues. IABP support was slowly reduced and removed after 4 days. After an extended stay in hospital, patient was discharged and went home. He is doing well after 1 year of follow up without any further cardiac issues.
Note: Right treatment at the right time is very important to give a good fighting chance for patients.
 A 45 year old gentleman presented to the emergency room with sudden onset of breathlessness. He had been otherwise healthy in the past. In the emergency room, it was noted that he had undertaken a long journey and was practically immobile during the travel. His pulse rate was high, and his oxygen saturation was only 84%.
A 45 year old gentleman presented to the emergency room with sudden onset of breathlessness. He had been otherwise healthy in the past. In the emergency room, it was noted that he had undertaken a long journey and was practically immobile during the travel. His pulse rate was high, and his oxygen saturation was only 84%.
Due to the history of prolonged immobilization, a condition known as pulmonary embolism was suspected. An ECG was obtained, that ruled out a heart attack. Echocardiography test was done and it suggested that the pressure in the right-sided heart chambers (Right atrium and right ventricle) were elevated (Picture of dilated RA/RV on echo).
CT scan of the pulmonary arteries was performed and it confirmed that there was a blood clot in the main pulmonary artery, confirming the diagnosis of pulmonary embolism (Picture of PA thrombus).
The patient was admitted to the ICU, an infusion of a clot-buster medication (Alteplase – a thrombolytic drug), was started. With this the patient’s symptoms quickly resolved. His oxygen saturation became normal and in the next 48 hours, the pressure in the right atrium and ventricle also normalized. The patient was put on blood thinner tablets for 3 months and discharged.
Pulmonary Embolism:
Pulmonary arteries carry impure blood from the right ventricle into both the lungs for purification.
In pulmonary embolism, a clot in the pulmonary arteries causes resistance to flow of blood from the right ventricle into the lungs. This is a serious condition and sometimes, massive pulmonary embolism can even be fatal.
Most often, clots that are formed in the veins of the legs and thighs get lodged in the pulmonary artery after they travel via the heart. Deep Vein Thrombosis (DVT), or clot formation in the leg or thigh veins is often as a result of immobilization following a fracture, surgery for the knee, hip or pelvis or prolonged journey. IN some patients, the reason for DVT remains undetected.
Massive pulmonary embolism may have to be treated with surgery or with thrombolytic therapy. Eary detection and treatment may save lives of patients with this affliction.
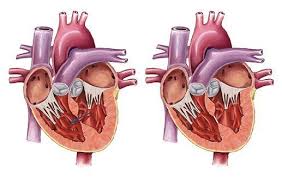 Ventricular septal defects (VSD) are holes in the wall between the two lower chambers (ventricles) of the heart. They can be present from birth (congenital) or rarely after a heart attack. Compared to the atrial septal defect (link for ASD here), congenital VSDs are detected earlier as they are symptomatic at an earlier age than ASDs.
Ventricular septal defects (VSD) are holes in the wall between the two lower chambers (ventricles) of the heart. They can be present from birth (congenital) or rarely after a heart attack. Compared to the atrial septal defect (link for ASD here), congenital VSDs are detected earlier as they are symptomatic at an earlier age than ASDs.
Symptoms in a baby include breathing difficulty, poor feeding, inadequate weight gain and recurrent chest infections. Occasionally bluish discoloration of the lips and skin is seen.
Smaller holes may close on their own although many require surgery or a catheter-based device closure. Device closure is a non-surgical procedure where a tube (catheter) is taken inside the heart from the blood vessels in the groin and a device is placed across the defect and the hole is closed. Surgery is usually needed in larger sized holes.
Hole in the heart: Ventricular septal defect
This is an echocardiogram image of a one-year-old child with weight gain issues. The mother said the child would not breast feed well and had recurrent chest infections. She did not notice any bluish discoloration of the skin or fainting spells.
He was found to be under weight for his age. On auscultation with a stethoscope, a murmur (abnormal heart sound) was heard. Echocardiogram revealed a hole in the wall (ventricular septum) separating right and left ventricles, the lower chambers of the heart. Medically such a hole is termed as ventricular septal defect (VSD).
 A 65-year-old patient who is Phd doctor went for a trek to Tiger mountain (a very tough vertical climb) in Bhutan without regular physical activity preceding the trip to prepare himself. He had a lot of chest discomfort associated with retro sternal burning after the climb, he thought it to be stomach upset, attributed it to exotic food he was having in that country. Then he returned the same day to India as planned and directly came to hospital from the airport as chest discomfort was worsening further. On arrival, he was diagnosed with evolved heart attack and was advised emergency coronary angioplasty. The same was completed successfully but he was told he has narrowing in another artery which may require similar procedure later. Patient made good recovery and was discharged in two days. As the Covid pandemic set in, he was reluctant to come to hospital to get the next procedure. Unfortunately, he had another heart attack due to the other narrowing, luckily he presented early to hospital and coronary angioplasty was done for the other narrowing with a stent. He is doing well with more than 9 months follow up.
A 65-year-old patient who is Phd doctor went for a trek to Tiger mountain (a very tough vertical climb) in Bhutan without regular physical activity preceding the trip to prepare himself. He had a lot of chest discomfort associated with retro sternal burning after the climb, he thought it to be stomach upset, attributed it to exotic food he was having in that country. Then he returned the same day to India as planned and directly came to hospital from the airport as chest discomfort was worsening further. On arrival, he was diagnosed with evolved heart attack and was advised emergency coronary angioplasty. The same was completed successfully but he was told he has narrowing in another artery which may require similar procedure later. Patient made good recovery and was discharged in two days. As the Covid pandemic set in, he was reluctant to come to hospital to get the next procedure. Unfortunately, he had another heart attack due to the other narrowing, luckily he presented early to hospital and coronary angioplasty was done for the other narrowing with a stent. He is doing well with more than 9 months follow up.
Note: Unaccustomed physical activity can lead to plaque rupture and heart attacks. Hence advised to follow graded exercise regimen always to prevent this kind of events.