HEART-FAILURE
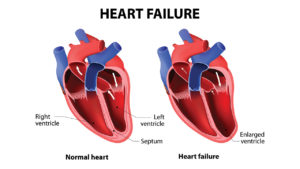 Heart failure means that the heart isn’t pumping as efficiently as it should. It does not mean that the heart has stopped working. Patients with heart failure may require medicines and other forms of treatment to help the heart function better and to remain free from symptoms.
Heart failure means that the heart isn’t pumping as efficiently as it should. It does not mean that the heart has stopped working. Patients with heart failure may require medicines and other forms of treatment to help the heart function better and to remain free from symptoms.
Heart muscle is sometimes too weak and cannot pump blood to the rest of the body with enough force (systolic failure). Sometimes it becomes stiff and has trouble in relaxation and can’t fill with enough blood (diastolic failure). Systolic and Diastolic heart failures sometimes co-exist.
The symptoms may present suddenly (acute) or progress gradually over a period of time (chronic).
- Heart failure with reduced left ventricular function (HF-rEF)
- Heart failure with preserved left ventricular function (HF-pEF)
Symptoms:
Symptoms of heart failure are mainly due to fluid accumulation in the lungs, legs, abdomen etc. Shortness of breath, excessive tiredness, swelling in the ankles, feet, legs, abdomen, rapid weight gain and frequent urination are commonly seen. Some people have shortness of breath and cough while lying flat.
Causes:
Previous heart attack, blocks in the arteries of the heart (Ischemic heart disease), High blood pressure, Diabetes, Valve disease, Congenital heart disease, Cardiomyopathy, Myocarditis (infection of the heart), Certain chemotherapy drugs, Hypo/hyper thyroidism, Alcohol or illicit drug usage, Obesity etc are some of the causes of Heart failure.
It is more common in:
- People who have had a heart attack. Damage to the heart muscle from a heart attack and can weaken the heart muscle.
- People who are aged 65 or older. Aging can weaken the heart muscle.
- Indians and Afro-Americans are more likely to have heart failure than people of other races and more likely to have symptoms at a younger age.
- People who are overweight. Excess weight puts strain on the heart. Being overweight also increases risk of heart disease and type 2 diabetes.
Diagnosis and treatment:
Heart Failure is usually detected after a complete review of the medical history, physical examination, and results from blood and/or cardiac imaging tests.
ECG, Chest X ray and Echocardiogram are usually performed to diagnose heart failure.
Stress testing (TMT, Radionuclide scans or Stress echocardiography) or Cardiac MRI may be advised in some cases. Coronary angiography and cardiac catheterisation is advised in select cases.
Blood tests to rule out anemia, kidney and thyroid disorders are also performed. Specific tests like BNP (Brain Natriuretic Peptide) are done in a patients with suspected heart failure for diagnosis and to assess prognosis.
How to manage heart failure?
Early diagnosis and treatment can help people with heart failure live longer and more active lives. Treatment includes a combination of lifestyle changes, medications, cardiac rehabilitation, and cardiac procedures.
Adopting a healthy lifestyle should be topmost priority. Avoiding excessive salt consumption, regular exercise, avoiding smoking, alcohol, and illicit drugs usage, maintaining healthy weight, monitoring fluid intake and restricting liquids where necessary, managing co-existing conditions such as high blood pressure, diabetes, chronic kidney disease are all part of holistic treatment of heart failure.
A combination of medications is typically used to reduce symptoms and to prevent worsening of heart failure. These include drugs that reduce the fluid accumulation (“water pills”) and those that can improve the efficiency of the heart when taken over long periods of time. Commonly used drug groups are: Diuretics, ACE inhibitors, Angiotensin receptor blockers,
Angiotensin Receptor/Neprilysin Inhibitors, Beta blockers and Mineralocorticoid Receptor antagonists.
Invasive Treatment for Heart Failure:
Coronary angiography to detect blocks and treatment by stents or bypass surgery may be performed in some cases of heart failure. Repair or replacement of diseased heart valves may help improve heart failure.
Some people can have very rapid, irregular heartbeats (arrhythmias) which can lead to sudden cardiac arrest. A device called Implantable cardioverter defibrillator (ICD) is implanted which checks the heart rate and uses electrical pulses to correct irregular heart rhythm.
In advanced stages of heart failure, the right and left sides of the heart may no longer contract at the same time. This disrupts the heart’s pumping. To correct this problem, a device called Cardiac resynchronization therapy (CRT) is implanted. This device helps both sides of the heart contract at the same time, which can decrease heart failure symptoms.
Newer therapies like Cardiac Contractility Modulation (CCM) offers hope by enhancing both the strength of ventricular contraction and the heart’s pumping capacity.
People who have severe heart failure symptoms at rest, despite medications and devices, may need:
- A mechanical heart pump, such as a left ventricular assist device (VAD). This device helps pump blood from the heart to the rest of the body. The long-term VAD can be used as a bridge to transplant as well as destination therapy for patients who are not candidates for heart transplant.
- During a heart transplant, a person’s diseased heart is replaced with a healthy heart from a deceased donor. Heart transplants are done as a life-saving measure for end-stage heart failure when medications, devices and surgery have failed.
Cardiac Rehabilitation:
Cardiac rehabilitation is a medically supervised program to improve the fitness level and health needs. This program includes exercise counselling and training as well as provides a support system to help adopt lifelong healthy behaviours and monitor progress.